Imagine a quiet afternoon. You’re feeling fine, perhaps a little tired, but nothing alarming. Then, you receive a gentle nudge from your doctor’s office: “It’s time for your annual physical, and we’d like to include a routine heart health checkup.” Suddenly, a wave of uncertainty, maybe even anxiety, washes over you. What exactly does that entail? Will they find something? What should you even do to prepare?
You’re not alone in these feelings. The prospect of any medical examination, especially one focusing on something as vital as your heart, can be daunting. But understanding what a heart health checkup involves and how to prepare can transform that apprehension into empowerment. This comprehensive guide will walk you through the process, offering clarity, practical advice, and the reassurance you need to approach your checkup with confidence.
The Silent Threat: Why Proactive Heart Health Matters More Than Ever
Cardiovascular disease (CVD) remains the leading cause of death globally, claiming millions of lives each year. In the United States alone, someone has a heart attack every 40 seconds. These aren’t just statistics; they represent families, futures, and dreams cut short. What makes heart disease particularly insidious is its often silent progression. Conditions like high blood pressure or elevated cholesterol, often referred to as “silent killers,” can develop over years without noticeable symptoms, slowly damaging your arteries and heart muscle until a critical event occurs.
The impact extends far beyond individual health. Heart disease places immense strain on healthcare systems, leads to significant economic burdens through lost productivity, and diminishes the quality of life for survivors and their caregivers. For the individual, living with advanced heart disease can mean chronic pain, shortness of breath, limited mobility, and a constant shadow of fear. This is precisely why early detection is not merely a recommendation but a critical act of self-preservation. A proactive heart health checkup can identify risk factors before they escalate into serious problems, offering a crucial window for intervention and prevention.
[Suggestion for image: Infographic showing global/national heart disease statistics, with a visual representation of “silent killer” conditions like high blood pressure/cholesterol.]
What Exactly Is a Heart Health Checkup? Understanding Its Purpose
A heart health checkup, often integrated into a general physical, is a series of evaluations designed to assess your cardiovascular risk factors and the overall health of your heart. It’s not just about looking for existing disease but also identifying potential future problems. The goal is to give you and your doctor a clear picture of your heart’s current status and to develop a personalized plan to maintain or improve its health.
These checkups typically involve a combination of:
- Review of Medical and Family History: Understanding your past health and genetic predispositions.
- Physical Examination: Assessing key vital signs and physical indicators.
- Blood Tests: Measuring critical markers that indicate risk.
- Diagnostic Tests: Occasionally, more specific tests might be ordered based on initial findings.
By bringing all this information together, your doctor can estimate your risk of developing heart disease, a heart attack, or a stroke in the coming years. This comprehensive approach empowers you with knowledge, allowing you to take charge of your cardiovascular well-being.
Why Early Detection Matters Immensely for Your Heart
The benefits of identifying heart disease risk factors early are profound and scientifically well-documented. Catching issues like high blood pressure, high cholesterol, or pre-diabetes before they lead to significant heart damage can literally be life-saving. For instance, managing hypertension effectively in its early stages can prevent heart failure, kidney disease, and stroke.
Consider the case of Maria, a 52-year-old marketing executive. She felt perfectly fine, but during a routine heart health checkup, her doctor noted consistently elevated blood pressure readings and a lipid panel showing high LDL (“bad”) cholesterol. Maria was initially resistant to medication, but her doctor explained the long-term risks, citing data from the Centers for Disease Control and Prevention (CDC), which highlights that about half of all Americans have at least one of three key risk factors for heart disease: high blood pressure, high cholesterol, and smoking. Armed with this knowledge and a clear understanding of her personal risk, Maria committed to lifestyle changes—a Mediterranean diet, daily walks—and started low-dose medication. Five years later, her blood pressure and cholesterol are well-managed, and she’s enjoying an active life, likely having averted a much more serious health crisis.
Early detection allows for:
- Timely Interventions: Lifestyle modifications, dietary changes, and sometimes medication can begin before irreversible damage occurs.
- Improved Prognosis: Many heart conditions, when caught early, are highly manageable, leading to a better quality of life and increased longevity.
- Reduced Healthcare Costs: Preventing a heart attack or stroke is far less costly, both financially and emotionally, than treating one.
- Peace of Mind: Knowing your heart’s status, even if it requires action, is better than living with uncertainty.
[Suggestion for image: A timeline graphic illustrating the progression of heart disease and points of early intervention.]
Preparing for Your Heart Health Checkup: A Step-by-Step Guide
Approaching your heart health checkup prepared not only streamlines the process but also ensures you get the most accurate and useful information. Here’s how to get ready:
Before Your Appointment: Gathering Vital Information
- Document Your Medical History:
- Current Medications: Make a list of all prescriptions, over-the-counter drugs, vitamins, and supplements you take, including dosages.
- Past Medical Conditions: Note any previous diagnoses, surgeries, or chronic conditions.
- Allergies: List any known allergies to medications, foods, or environmental factors.
- Understand Your Family History: Heart disease often runs in families. Know if your parents, siblings, or grandparents had heart attacks, strokes, high blood pressure, high cholesterol, or diabetes, and at what age they developed these conditions. This information is crucial for assessing your genetic predisposition.
- Note Down Your Symptoms (If Any): Even seemingly minor symptoms like occasional shortness of breath, chest discomfort during exertion, unusual fatigue, or swelling in your legs can be important clues. Be specific about when they occur, how long they last, and what makes them better or worse.
- Prepare Your Questions: Write down any questions or concerns you have. This ensures you don’t forget anything important during the consultation. Examples include:
- “What are my personal risk factors for heart disease?”
- “What lifestyle changes can I make to improve my heart health?”
- “Do I need any specific tests beyond the routine ones?”
- “How often should I have these checkups?”
- Check Fasting Requirements: Many blood tests, especially those for cholesterol and blood sugar, require you to fast for 8-12 hours beforehand. Confirm this with your doctor’s office when you schedule the appointment.
The Day of Your Appointment: Practical Tips
- Wear Comfortable Clothing: You may need to have your blood pressure taken on your arm, and potentially an ECG (electrocardiogram) which involves placing electrodes on your chest and limbs. Loose, comfortable attire helps.
- Stay Hydrated (Unless Fasting): If not fasting, drink plenty of water. If fasting, only water is usually permitted.
- Bring Your List of Questions and Notes: Don’t rely on memory. Having everything written down ensures a productive conversation.
- Be Honest and Open: This is crucial. Your doctor can only help you effectively if they have a complete and accurate picture of your health habits, concerns, and history. Don’t withhold information out of embarrassment or fear.
Common Tests You Might Encounter During a Heart Exam
During your checkup, your doctor will likely perform several standard assessments:
- Blood Pressure Measurement: This measures the force of your blood against the walls of your arteries. High blood pressure (hypertension) is a major risk factor for heart disease and stroke.
- Lipid Panel (Cholesterol Test): A blood test that measures your total cholesterol, LDL (low-density lipoprotein, “bad” cholesterol), HDL (high-density lipoprotein, “good” cholesterol), and triglycerides. These levels indicate your risk of plaque buildup in your arteries.
- Blood Glucose Test: Measures your blood sugar levels. High glucose levels can indicate pre-diabetes or diabetes, another significant risk factor for heart disease.
- Body Mass Index (BMI) and Waist Circumference: These measurements help assess obesity, which is closely linked to cardiovascular risk.
- Electrocardiogram (ECG or EKG): A non-invasive test that records the electrical signals of your heart. It can detect arrhythmias (irregular heartbeats), signs of past heart attacks, or other heart conditions.
- Other Tests (If Indicated): Depending on your risk factors and initial findings, your doctor might recommend further tests such as an echocardiogram (ultrasound of the heart), stress test (to see how your heart performs under exertion), or advanced imaging.
[Suggestion for image: A diagram explaining what an ECG measures, or a chart showing healthy vs. unhealthy ranges for blood pressure and cholesterol.]
Understanding Your Results: What Do the Numbers Mean?
Receiving your test results can feel like deciphering a secret code. Your doctor will explain everything, but having a basic understanding empowers you to engage more actively in your health management. For example, regarding blood pressure, a reading of 120/80 mmHg is generally considered normal. Readings consistently above this, especially 130/80 mmHg or higher, warrant attention. For cholesterol, the American Heart Association (AHA) provides clear guidelines, with an optimal LDL cholesterol typically below 100 mg/dL and HDL cholesterol ideally 60 mg/dL or higher. These numbers are benchmarks, and your individual target ranges may vary based on your overall health and other risk factors.
Don’t hesitate to ask your doctor to explain any results you don’t understand. Ask what each number means for your personal risk and what specific steps you can take to improve them. This collaborative approach is key to effective health management.
Beyond the Exam Room: Sustaining Heart Health
A heart health checkup is a snapshot; true heart health is a continuous journey. The insights gained from your checkup should be a springboard for sustained lifestyle choices. Evidence-based strategies for long-term cardiovascular well-being include:
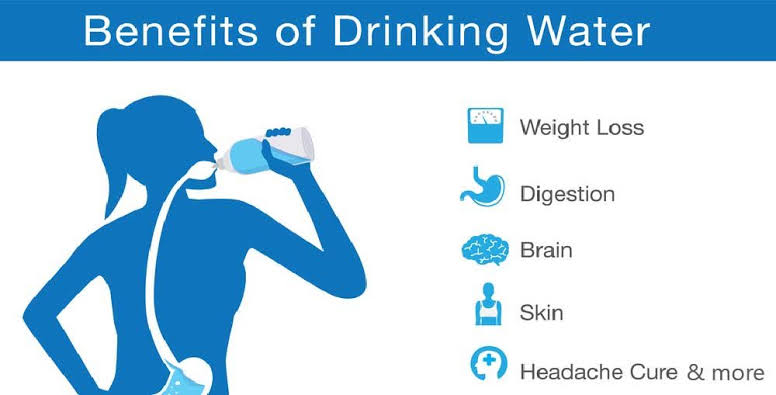
- Adopt a Heart-Healthy Diet: Focus on whole, unprocessed foods. Emphasize fruits, vegetables, whole grains, lean proteins, and healthy fats (like those found in olive oil, avocados, and nuts). Limit saturated and trans fats, added sugars, and excessive sodium.
- Engage in Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise per week, combined with muscle-strengthening activities on two or more days. Even short bursts of activity add up.
- Maintain a Healthy Weight: Achieving and maintaining a healthy BMI (Body Mass Index) significantly reduces the burden on your heart.
- Manage Stress Effectively: Chronic stress can contribute to high blood pressure and unhealthy coping mechanisms. Incorporate stress-reduction techniques like meditation, yoga, deep breathing exercises, or spending time in nature.
- Prioritize Quality Sleep: Poor sleep patterns can impact blood pressure and hormone regulation. Aim for 7-9 hours of quality sleep per night.
- Quit Smoking: If you smoke, quitting is the single most impactful step you can take for your heart health. Smoking dramatically increases your risk of heart attack and stroke.
- Limit Alcohol Intake: If you drink alcohol, do so in moderation (up to one drink per day for women, up to two for men).
These strategies aren’t just recommendations; they are clinically proven pathways to a healthier heart, often forming the first line of defense against cardiovascular disease, as highlighted by the National Heart, Lung, and Blood Institute (NHLBI).
What Few People Tell You About Heart Health Checks
While the clinical aspects of a heart health checkup are well-documented, there are often less obvious, but equally important, facets that few discuss:
- The Emotional Rollercoaster: It’s perfectly normal to feel anxious before and during the checkup, and even a sense of relief or worry after receiving results. Acknowledging these emotions can help you process them. Discuss any significant fears with your doctor or a trusted friend/family member.
- Variability in Readings: A single high blood pressure reading doesn’t automatically mean you have hypertension. Many factors can influence a reading (e.g., “white coat syndrome,” stress, recent caffeine intake). Your doctor will look for consistent patterns over time and may recommend at-home monitoring for a more accurate picture.
- It’s a Conversation, Not an Interrogation: Your doctor wants to help you. Don’t view the appointment as a test you can fail. It’s an opportunity for a collaborative discussion about your health. Ask questions, voice concerns, and actively participate in decisions about your care. As Dr. Anya Sharma, a cardiologist focusing on preventive care, often advises, “Your heart health journey is a partnership. Your role in asking questions and advocating for yourself is just as vital as our role in providing expert guidance and care.”
- The “Normal” Trap: Receiving “normal” results is great, but it doesn’t grant immunity. Lifestyle choices still matter. And conversely, slightly elevated readings don’t mean imminent doom; they’re often a powerful prompt to make manageable, impactful changes.
- The Long-Term Perspective: A heart health checkup isn’t a one-and-done event. It’s part of an ongoing dialogue with your body and your healthcare provider. Regular checkups, even when you feel well, establish a baseline and allow for early detection of subtle changes over time, which are often more telling than a single reading.
Understanding these nuances can help you approach your checkup with a more holistic and realistic mindset.
Your Journey to a Stronger Heart Starts Here
Taking charge of your heart health begins with knowledge, preparation, and proactive engagement. A heart health checkup isn’t just a medical appointment; it’s an invaluable opportunity to understand your body better, mitigate risks, and invest in a longer, healthier future. Embrace it as a powerful step towards well-being, recognizing that every small effort you make now contributes to a lifetime of vitality. Don’t wait for symptoms to emerge; empower yourself with the information and tools to protect your most vital organ. Schedule your comprehensive heart health checkup today, and embark on a path to a stronger, healthier heart.
***
Author Bio
Dr. Eleanor Vance is a seasoned health writer and public health advocate with a passion for preventive medicine. Holding an M.D. from the University of California, San Francisco, and a Master’s in Public Health from Johns Hopkins University, she brings a wealth of clinical knowledge and a deep understanding of evidence-based health practices to her work. Dr. Vance has contributed to numerous health education initiatives and has a particular focus on empowering individuals through clear, actionable health information, especially in the realm of cardiovascular wellness and chronic disease prevention.